Transforming Lives: Deceased Donor Liver Transplantation in Bangalore
Deceased Donor Liver Transplant (DDLT)
When a patient does not have a family member who can donate a liver, the only option way to obtain a liver is through a deceased or brain death (cadaveric) donor. This type of transplant is referred to as a Deceased Donor Liver Transplant (DDLT).
In Deceased Donor (Cadaveric) Liver Transplant liver comes from people who have died suddenly, usually from an accident or bleed into the brain. Their heart is still beating,
but their brain has stopped working so they’re considered legally dead. The donor is usually in an intensive-care unit. These individuals are usually been relatively healthy before their death. These people have previously expressed to their families a willingness to donate their organs, or their families have made the decision to donate their organs so that someone else will have a chance to live a better life.
After consent from relatives, retrieval procedure is performed in operation theatre. After removal from the donor (a process called liver retrieval), the liver can safely preserved outside the body in special preservation solutions for 6- 8 hours, which is why recipients are often called to the hospital at short notice based on availability of organ. All donors are screened for hepatitis viruses and the HIV to ensure that they don’t pose a health threat to the recipient.
Waiting List for Liver Transplant
Patients have to register themselves at Individual centers/NOTTO for cadaveric organ allocation in India. Once a liver is available and matches the patient’s blood group, they are called for a transplant based on their MELD score. Currently, India houses a state-based regulation for organ allocation based on the MELD score & waiting list.
What is a Deceased Donor Liver Transplantation
Deceased Donor Liver Transplantation in Bangalore, spearheaded by renowned Liver transplantation doctor in Bangalore Dr. Rajiv Lochan, is a life-saving surgical procedure performed to replace a diseased or failing liver with a healthy liver obtained from a deceased donor. This type of transplantation is typically considered when a patient’s liver function has severely deteriorated due to conditions such as liver cirrhosis, liver cancer, or acute liver failure, and other treatment options have been exhausted.
The process begins with the identification of a suitable deceased donor whose liver matches the recipient’s blood type and other compatibility factors. Once a suitable donor is found, the liver is procured through a meticulous surgical procedure while maintaining its viability.
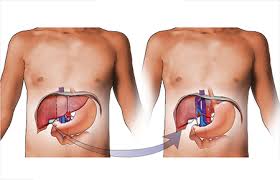
The liver is then preserved and transported to the transplant centre for transplantation into the recipient. Before the transplant surgery, the recipient undergoes thorough evaluation to assess their overall health and suitability for the procedure. During the liver transplant surgery, the recipient’s diseased liver is removed, and the healthy donor liver is implanted. Following the surgery, the recipient requires lifelong immunosuppressive medication to prevent rejection of the transplanted organ. Deceased Donor Liver Transplantation offers a chance for patients with end-stage liver disease to regain normal liver function and significantly improve their quality of life. However, it is a complex procedure with potential risks and complications, requiring close monitoring and ongoing medical care post-transplantation.
